Research Snippet #1: Probes to Localise Metastases of Ovarian Cancer
Welcome to CSM’s first research post for 2020.
Through the rest of the year, I will be writing about some of the latest papers on cutting-edge cancer research. Following up on our recent seminar on gynaecological oncology, let’s look at an interesting new paper from that field, which introduces a new method that could potentially transform the way imaging is used to direct surgery for metastatic ovarian cancer.
The paper we will be looking at is titled “Gonadotrophin-releasing hormone receptor-targeted near-infrared fluorescence probe for specific recognition and localisation of peritoneal metastases of ovarian cancer,” by Liu et al. and published in the journal Frontiers in Oncology on February 28 2020.[1] Currently, for patients diagnosed with stage III or IV ovarian cancer, the 10-year survival rate is only 15%, and the main treatment for advanced ovarian cancer is surgery.[2] This surgery is guided by traditional imaging, such as ultrasound, CT and MRI.
The authors of this study investigated a new alternative way of guiding this surgery. They studied the gonadotrophin-releasing hormone receptor (GnRHR) as a marker for visualising metastases of ovarian cancer in the peritoneum. This fluorescence imaging has the potential to make it much easier to distinguish cancerous from normal tissue before, during and after surgery, and so to transform the effectiveness of surgical removal of metastases. Liu et al. found that attaching an infrared fluorophore to a GnRHR agonist (a molecule which, like gonadotrophin-releasing hormone, binds to the GnRHR) creates a probe that can effectively bind specifically to GnRHR-positive ovarian cancer cells. This raises the hope that such a technique can be used to make surgical treatment more effective in future.
How was this research done? Liu et al. first analysed the transcriptome profiles of ovarian cells that are databased and found that 97.5% of breast cancers, 79.1% of endometrial cancers, and 97.1% of prostate cancers and, importantly, 95% of high-grade ovarian cancers, expressed GnRHR at high levels. They then conjugated an indocyanine green (ICG) fluorescent dye to a GnRHR agonist (GnRHa) to create a probe (GnRHa-ICG) that can target the GnRHR molecule and release a fluorescent signal. They incubated ovarian cancer cell lines with this probe, confirming that this probe binds successfully to ovarian cancer cells, which we can see in Liu et al.’s microscopy images (see figure 1).
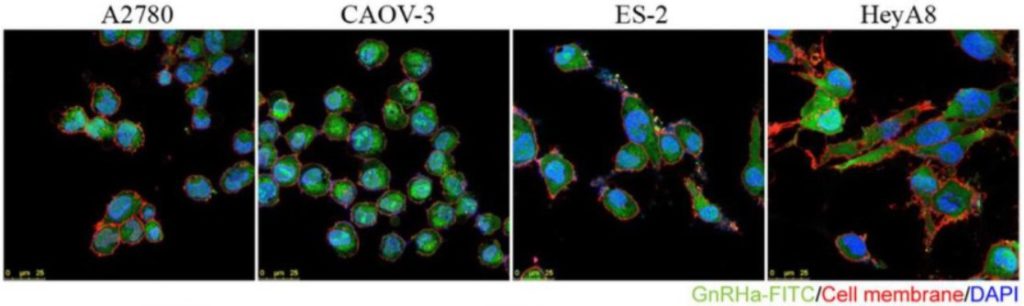
Figure 1: fluorescence microscopy images from Liu et al. showing the fluorescent probe (green) binding to ovarian cancer cells (blue and red).
Following this, Liu et al. applied this study to larger-scale imaging of entire tissues, to test whether this fluorescence could be used to locate metastases. To do this, they used a mouse model of metastatic ovarian cancer and injected the GnRHa-ICG probe into the mouse peritoneum. The same was done with a set of controls without ovarian cancer. Two hours later, imaging was performed on the mouse mesentery, omentum and intestine—three common sites for ovarian cancer metastases. The results (see figure 2) demonstrated that the probe could indeed be used to provide fluorescence imaging of the metastases.
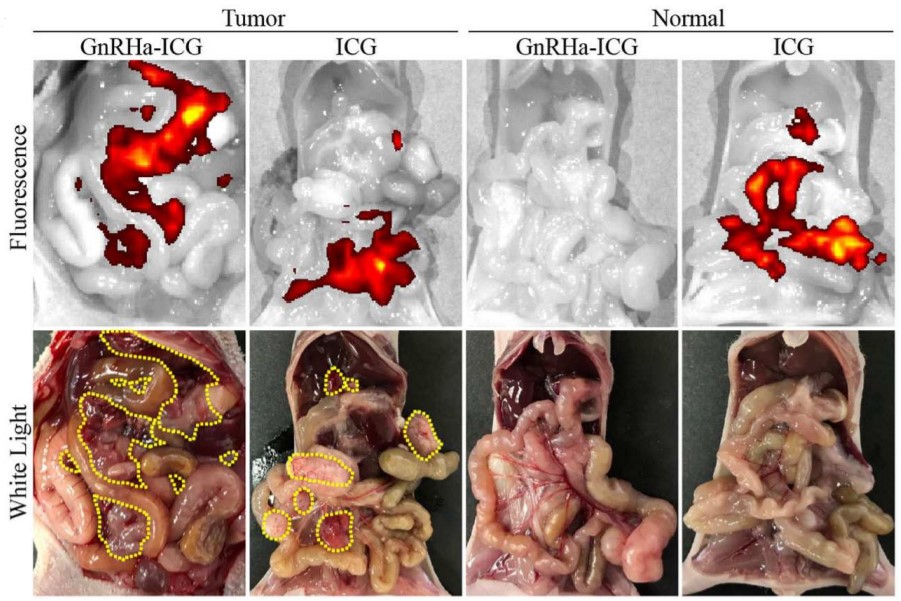
Figure 2: Images of the peritoneal cavity of mice two hours after the injection of the GnRHa-ICG probe in mice with (“tumour”) and without (“normal”) metastatic ovarian cancer. The fluorescent signal from the probe is overlayed in the fluorescence images (top row). In the photographs under white light (bottom row) the true outlines of the metastases are indicated in yellow. The images labelled “ICG” were taken for comparison with injection of an ICG fluorescent marker not coupled with a GnRHa agonist, which thus lacks any specific binding capacity.
Looking at the images above, we see a close, though not perfect, correlation between the actual sites of metastases and the fluorescent signals from the probe. We can appreciate how using this imaging in conjunction with surgery can allow surgeons and oncologists to distinguish much more easily between metastatic cancer cells and normal cells of the peritoneum. Such imaging techniques mean that, in future, it could become much easier to detect and remove all metastases during surgery, many of which may otherwise be missed.
Resources:
- Liu, Q., et al., Gonadotropin-Releasing Hormone Receptor-Targeted Near-Infrared Fluorescence Probe for Specific Recognition and Localization of Peritoneal Metastases of Ovarian Cancer. Frontiers in Oncology, 2020. 10: p. 266.
- Narod, S., Can advanced-stage ovarian cancer be cured? Nature Reviews Clinical Oncology, 2016. 13: p. 255-261.