Research Snippet #2: Impact of COVID-19 on Oncology Patients
It’s time for the second CSM research article for 2020.
Given that we’re now in the midst of the dreaded second wave of the COVID-19 pandemic, I thought it would be a good time to consider how the pandemic has impacted some of the most vulnerable members of our society; cancer patients. To do this, we will look at Joode et al.’s recent paper “Impact of the coronavirus disease 2019 pandemic on cancer treatment, the patients’ perspective,” which studied the impact of the pandemic from the perspective of cancer patients throughout the Netherlands.[1] The study began on March the 29th and was published on the 16th of June, and was the first study to be undertaken specifically from the perspective of patients rather than doctors.
The reason we are so concerned about cancer patients is that they are at increased risk not only of catching COVID-19, but also of having more severe disease.[2] On top of this, there are iatrogenic factors that contribute to their vulnerability; chemotherapy regimens are immunosuppressive and further increase this risk, while many cancer treatments do not allow patients to remain isolated and safe, since they necessitate going into hospital. The other problem is patients avoiding the hospital due to fears of contracting COVID-19, and this would be the case for 19% of patients who were surveyed, whereas 75% of patients would say their behaviour towards going to the hospital was unchanged by the pandemic.
Joode et al. designed a survey which was conducted nation-wide throughout the Netherlands, asking 5,302 cancer patients about their experiences during the pandemic, usually by an in-person, by telephone or by video consultation with the patient. The study was carried out over a three-week period. In their survey, they divided the patients into groups according to whether their cancer was incurable, curable or cured. As we see in the graph below, they compared the number of patients in each category who:
Required hospital contact for their treatment (dark blue); something which limits the ability of patients to socially isolate, leading to a higher risk of contracting COVID-19.
Stated they had already experienced consequences from COVID-19 (red); these are patients who had experienced changes to their consultations, treatment, and follow-up due to the pandemic.
Stated they had not yet experienced consequences from COVID-19 (yellow)
Had not experienced any consequences from COVID-19 (dark green); patients whose treatment was and would remain entirely unchanged by COVID-19.
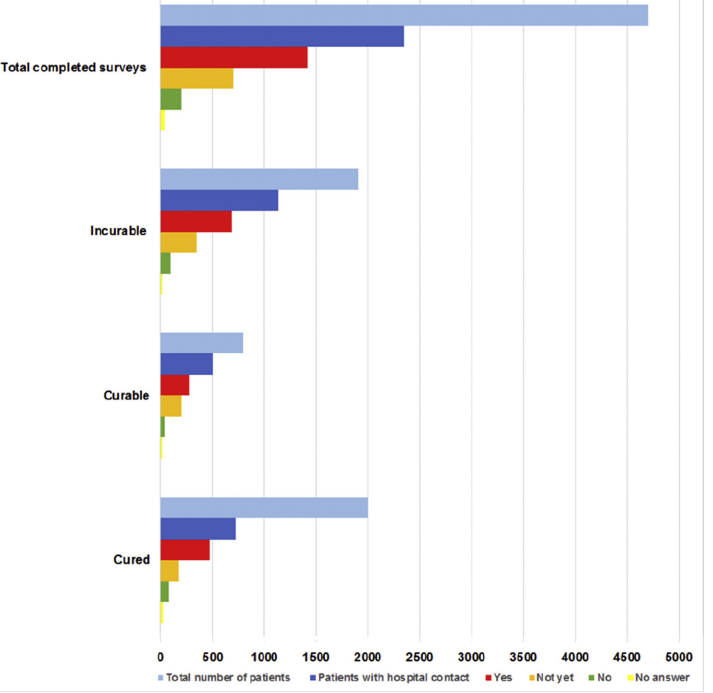
Figure 1: Graph from Joode et al. showing responses to the question of whether they had experienced consequences from the COVID-19 pandemic, sorted according to whether their cancer was ‘incurable’, ‘curable’ or ‘cured’.
As we can see here, few patients could say that the pandemic had not affected their treatment in some way, except for the group of patients who had already been cured. The authors found that most of the changes (more than 79%) had been initiated by the hospital rather than the patient. The changes were mostly the conversion of in-person consultations to telehealth, and the treatment itself was affected in 3% of patients who were awaiting treatment, and 7% of patients who were already under treatment. In 20% of these patients, this meant an adjustment of the treatment itself, while in the rest of the patients it meant a delay of treatment or discontinuation of treatment. In good news, the majority of patients (> 72%) reported that they were adequately informed by the hospital about why the treatment changes were necessary.
Patients were also asked if they were concerned about whether the pandemic would adversely affect their cancer treatment or follow-up. Many patients were concerned, particularly those who had experienced a delay (55%) or discontinuation (62%) of treatment. Concerning the virus itself, 47% of patients reported being “very concerned” about the possibility of being infected with COVID-19). It was also observed that the proportion of patients who were very concerned was highest amongst those with incurable disease compared with those whose disease was curable or cured.
The main takeaway from this study is that, in general, oncology patients are very concerned about the impact of the pandemic on their treatment and follow-up, particularly those with incurable disease, who are most vulnerable. Joode et al. finished by recommending that all cancer patients would benefit from additional psycho-oncological support and information, as well as support for patients who are facing day-to-day consequences from the pandemic.
If you would like to find out more, here is a link to a copy of Joode et al.’s paper:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7334940/pdf/main.pdf
Resources:
- de Joode, K., et al., Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients’ perspective. European Journal of Cancer, 2020. 136: p. 132-139.
- Zhang, L., et al., Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Annals of Oncology, 2020. 31(7): p. 894-901.